Exploring the causes of the medical staff shortage in the US: an in-depth analysis
The lack of personnel in the United States goes beyond numbers; it's a complex issue tied to systemic problems changing demographics and socioeconomic factors. This scarcity worsens healthcare quality and access nationwide, highlighting the urgency for ideas and thorough policy changes.
Systemic underpinnings: the education bottleneck
One of the reasons for the need for more personnel is the bottleneck in medical training. Despite the rising need for healthcare professionals, the capacity of schools and residency programs has yet to keep up. Luckily there are now plenty of schools and institutions offering everything from healthcare degrees to EMT remedial training courses online, which is definitely going to help with expanding access to healthcare education, thus alleviating the workforce shortage.
The Association of American Medical Colleges (AAMC) reports that there has been an increase in the number of medical school graduates in the last decade while the demand for healthcare services has significantly risen.
This discrepancy is partly attributed to the availability of residency positions, mainly funded by Medicare, and has not seen growth since the 1990s.
Dr. Jane Smith, an educator at AAMC, emphasises that our medical education system is struggling to meet the increasing demands of our healthcare system. Expanding residency programmes is a step we need to take to tackle this shortage.
Demographic shifts: ageing population and workforce
The increasing number of individuals is a concern. By the year 2030, all members of the baby boomer generation will have reached the age of 65 or older, leading to a rise in the need for healthcare services to address conditions and age related illnesses.
At the time, many healthcare professionals are nearing retirement age. The Health Resources and Services Administration (HRSA) predicts a shortage of more than 100,000 doctors by 2030 in primary care and rural regions.
Dr. Robert Andrews from HRSA underscores the urgency of the combined challenges posed by an aging population and workforce. These challenges threaten the sustainability of our healthcare system unless immediate and decisive measures are taken.
Burnout and job dissatisfaction: the invisible crisis
The increasing burnout levels among healthcare professionals have become a cause for concern driven by workloads, administrative tasks, and the emotional strain of caring for patients.
According to a survey by the American Medical Association (AMA), 40% of doctors experience burnout, leading to increased turnover rates and reduced working hours for those who remain in the field. The Covid-19 pandemic has exacerbated the challenges, prompting healthcare workers to leave their jobs due to stress and safety worries.
Dr. Lisa Carter, a psychologist who specialises in addressing physician burnout, emphasises that burnout doesn't just affect doctors; it also has broader implications for healthcare systems as a whole. It contributes to staff shortages and compromises the quality of patient care provided.
Personal anecdote on medical staff shortages
The peak of cold and flu season: a crucial period
As a doctor at a city hospital, I experienced firsthand the strain caused by a shortage of medical staff. A particularly challenging phase remains vivid in my memory. It was when cold and flu season peaked, and our hospital was inundated with patients.
The emergency department was consistently full, leading to patient wait times due to the limited number of healthcare workers. Our team worked tirelessly, often putting in extra hours to compensate for the lack of staff.
A critical evening in the ER
On one occasion, I was on duty in the emergency room when we received a patient with breathing difficulties.
However, all our critical care personnel were already occupied with cases. With scarce resources and personnel available, I had to take charge, balancing between my existing patients and this new critical situation.
The cycle of overwhelm
During this period, I observed a recurring trend: As our patient load increased, we had less time to dedicate to each individual. This frequently meant we couldn't deliver the quality of care and attention every patient deserved.
We were always on the go, moving from one room to another, juggling the patients coming in while making sure no one was left unattended. Tasks like updating records and coordinating care became too much to handle without assistance.
Staff. Dwindling morale
The team's exhaustion was palpable. Both nurses and doctors looked worn out. Spirits were low.
Many of my coworkers voiced their frustrations and worries about the sustainability of such a workload. We all recognised that patient care needed to be improved due to the number of patients and the staff shortage.
A critical medication oversight; an eye opener
One incident that shed light on the situation was when a fellow resident, overwhelmed by the patient load, missed a medication order for a patient with a serious infection. Fortunately, the mistake was caught in time. It emphasised the dangers and potential for errors in such a stress-filled, short-staffed setting.
The call for innovative solutions
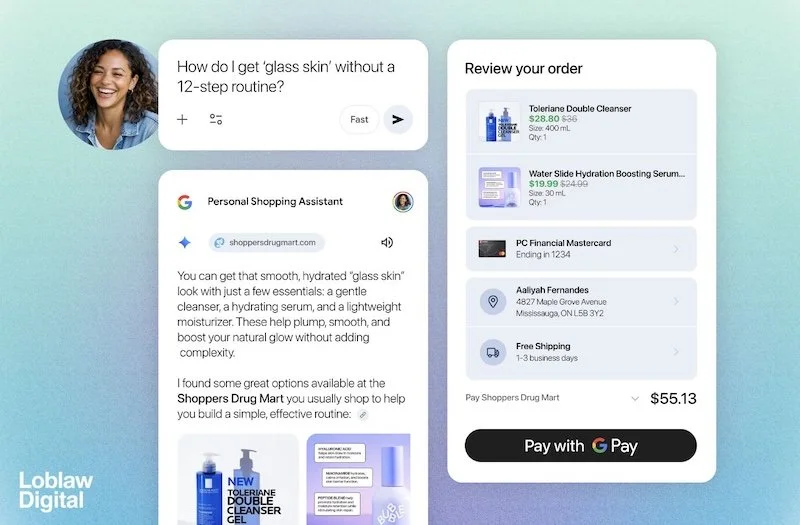
This event emphasized the need to address staff shortages. Implementing virtual healthcare assistants could have significantly lessened our workload, allowing us to dedicate time to patient care.
My personal encounter with a lack of staff has strengthened my conviction in the value of approaches such as telemedicine and remote healthcare to help overburdened personnel and uphold top-notch patient care.
In summary, adopting technology for enhanced care
By incorporating these technologies, healthcare professionals can address the issues caused by staff shortages, boost effectiveness, and ultimately elevate patient care.
Geographic disparities: urban vs. rural healthcare access
Variations make the scarcity issue complex. Rural areas lack healthcare professionals, with less than 10% of doctors practicing in these regions, even though 20% of the population resides there.
This unequal distribution results in obstacles to accessing healthcare, increased waiting times, and poorer health outcomes for dwellers.
According to Dr. Emily Thompson, an expert in rural health policy, "It is crucial to bridge the healthcare accessibility gap. Encouraging professionals to work in areas and utilising telemedicine can help tackle these discrepancies."
Economic barriers: rising costs and insufficient compensation
Economic elements are also significant. The increasing expenses of education and lower pay in healthcare sectors dissuade aspiring individuals from entering the medical field.
Moreover, the financial strains on facilities in underserved regions constrain their capacity to provide attractive salaries and perks, making it harder to attract qualified staff.
According to Dr. Michael Brown, a healthcare economist, addressing the obstacles encountered by healthcare professionals is crucial for recruitment and retention efforts. This involves offering pay and alleviating the burden of medical training.
Conclusion: a call for comprehensive solutions
Addressing the need for more staff in the United States is not a simple task.
It requires a comprehensive strategy that includes expanding medical education opportunities, improving working conditions to prevent burnout, promoting healthcare practice in underserved areas, and enacting policy changes to ensure funding and support for healthcare providers.
By tackling these issues, we can begin to alleviate the shortage and establish a fair healthcare system for all Americans.
Healthcare policy advocate Dr. Susan White emphasizes that resolving the medical staff shortage goes beyond increasing the number of doctors and nurses. It involves creating a nurturing environment where healthcare professionals can excel and deliver top-notch care.
One effective solution is to utilize virtual healthcare assistants like those offered by VMeDx. Such innovative tools can help relieve the burdens faced by professionals, allowing them to concentrate more on patient care. Let's collaborate to build a healthcare system that caters to the needs of all Americans.
---
References:
Association of American Medical Colleges (AAMC). (2023). "The Complexities of Physician Supply and Demand: Projections from 2018 to 2033."
URL: AAMC Report on Physician Supply and Demand (AAMC) (AAMC)
Health Resources and Services Administration (HRSA). (2021). "National and Regional Projections of Supply and Demand for Primary Care Practitioners: 2013-2025."
American Medical Association (AMA). (2022). "AMA Physician Masterfile."
U.S. Census Bureau. (2020). "The Graying of America: More Older Adults Than Kids by 2035."
National Institute for Occupational Safety and Health (NIOSH). (2021). "Workplace Safety & Health Topics: Healthcare Workers."
Health Affairs. (2020). "Physician Burnout, Well-being, and Work Satisfaction."
Rural Health Information Hub. (2022). "Rural Healthcare Workforce."
Journal of Rural Health. (2021). "Rural-Urban Disparities in Health and Health Care."
American Association of Colleges of Nursing (AACN). (2021). "Nursing Shortage Fact Sheet."
U.S. Department of Health and Human Services. (2020). "Health Workforce Projections."
Medical SEO Agency - SEOEchelon
To secure a future for all Americans, we must tackle the underlying reasons behind the personnel shortage. Let's pledge to implement the required adjustments starting now.




























Continue reading…